Recognizing the Early Warning Signs of Stomach Cancer
Stomach cancer can show early signs that shouldn't be ignored. Common symptoms include heartburn, nausea, and bloating. If these persist, seek medical advice. Early detection of stomach cancer improves outcomes. Regular check-ups can help identify potential issues before they advance.
Understanding Stomach Cancer
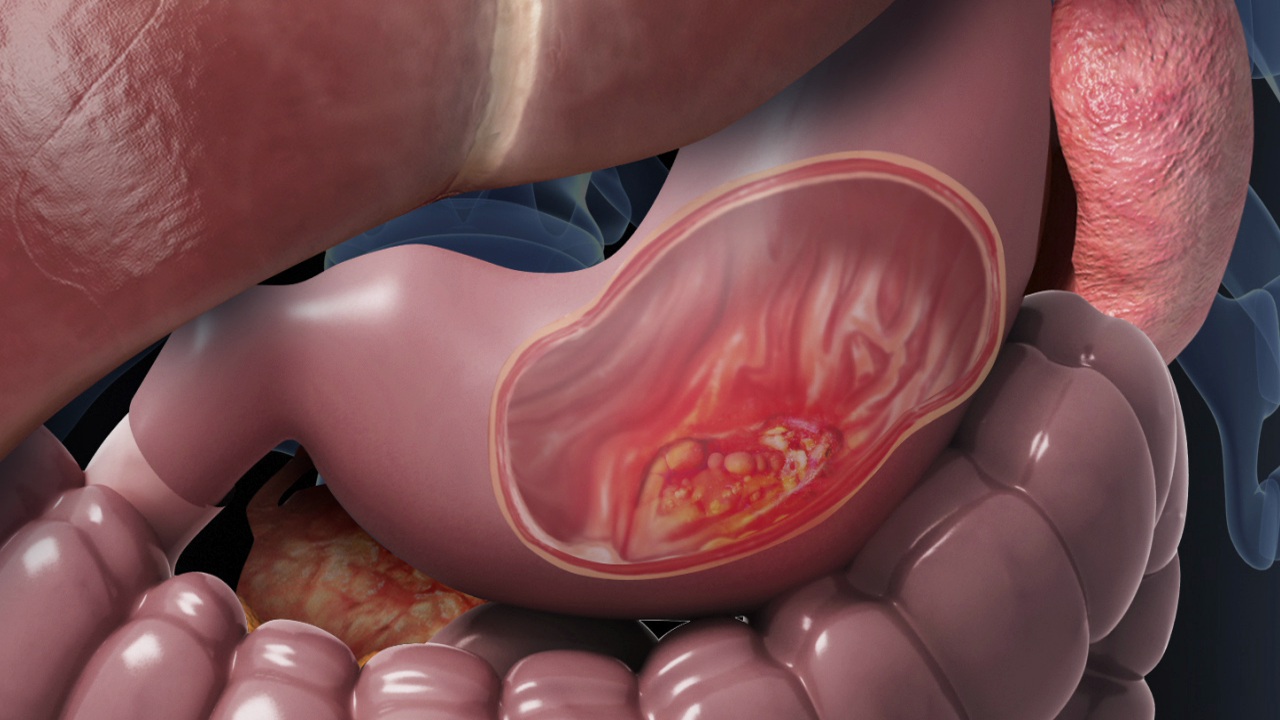
Stomach cancer, also known as gastric cancer, begins when cancerous cells form in the lining of the stomach. It's considered one of the most challenging cancers to detect early because initial symptoms often mimic other less serious conditions. The stomach is an essential component of our digestive system, and any interference in its function can lead to severe repercussions. Awareness, early diagnosis, and proactive management represent key aspects of dealing with stomach cancer. Understanding its signs, risk factors, and diagnostic procedures is vital for anyone looking to empower themselves and their loved ones to take preventative action.
Recognizing Early Indicators
With delayed symptom onset, the early stages of stomach cancer can often go unnoticed. Initial signs might include persistent indigestion, unexplained weight loss, or feeling bloated after meals. Despite the ambiguity of these symptoms, it's crucial to recognize potential alarm bells: chronic stomach pain, difficulty swallowing, and vomiting that persists over time. Many individuals may dismiss these as mere inconveniences, delaying professional evaluation. Emphasizing vigilance over one's bodily changes can lead to earlier intervention. If these signs persist over weeks or worsen, it is paramount to seek a healthcare provider for further analysis.
Common Symptoms of Progression
As stomach cancer progresses, the symptoms become more pronounced and direct. In addition to the aforementioned signs, more serious symptoms include severe nausea, blood in vomit or stools (which may appear dark and tarry), and a noticeable increase in fatigue. Some patients report feeling full after eating small amounts, indicative of the cancer's advancement impacting stomach capacity. These advancements can severely affect one's ability to maintain a healthy weight, meet nutritional needs, and perform daily activities. Awareness of these symptoms can prompt individuals to expedite medical consultation, allowing for therapeutic interventions.
Risk Factors in Focus
Understanding the risk factors associated with stomach cancer can lead to more informed lifestyle choices. Age is a significant factor, with those over 50 at higher risk. Diets rich in smoked, salted, or pickled foods can increase vulnerability, while low fruit and vegetable intake diminishes protective dietary effects. Smoking not only heightens gastric cancer risk but also exacerbates other health issues. Genetic factors also play a role; a family history of gastric cancer necessitates heightened awareness and possible genetic counseling. Awareness and modification of these risk factors can be instrumental in preventive measures.
Diagnostic Procedures and Screening
When symptoms indicative of potential stomach cancer manifest, a series of diagnostic tests can confirm the presence and extent of the disease. Endoscopic procedures are a primary form of examination, allowing physicians to visually assess the stomach's interior. Biopsies can provide definitive diagnoses by examining tissue samples. Imaging tests, including CT scans and PET scans, are also crucial in determining the cancer's spread. Regular screening for those with significant risk factors, before symptom onset, can be a life-saving step. An informed dialogue with a healthcare professional can guide appropriate testing strategies.
Path Forward: Treatment and Management
Treatment options for stomach cancer often depend on its stage and location, as well as the patient's overall health. Surgical solutions may include partial or total gastrectomy, aiming to remove cancerous growths. Chemotherapy and radiation can be part of a treatment regimen to target remaining cancerous cells. Innovations in therapies like targeted drugs and immunotherapy are expanding possibilities, offering hope for improved outcomes. Management doesn't end with treatment; it's an ongoing process that includes nutritional support and regular follow-ups to monitor recovery or detect recurrence. Empowering patients with comprehensive care and support systems is central to navigating a path forward.